Diet Plan for Gastric Bypass Patients
Table of Contents
- Pre-op Liquid Diet
- Post-op and Week 1
- Week 2 and 3
- Week 4 and 5
- Week 6
- How to Choose Gastric Bypass Appropriate Foods
- Recommended Gastric Bypass Diet/Recipe Books
Gastric bypass surgery is a lifesaving procedure. You will lose weight. You will reduce your co-morbidities. You will feel better and look better. However, to be successful (long-term), you have to change your diet.
This sounds simple, but it's not. Be prepared for a struggle. You've spent much of your life building and reinforcing bad eating habits. Those have to change.
Knowing what you can and can't eat is the first step towards a healthy diet. Your diet for the first five weeks after gastric bypass surgery is important for two reasons.
- Your safety. Eating the wrong food could put undue pressure on your healing stomach.
- Resetting your bad eating habits and replacing them with new healthy habits.
Pre-Op Liquid Diet
In order to reduce the amount of fat around the liver and spleen, a preoperative liquid diet must be followed 7-14 days before gastric bypass surgery. If this diet is not followed, then surgery may be delayed or canceled intra-operatively (during the procedure).
I can't stress enough how important it is to follow the pre-op diet. You've likely waited 6 months to a year to get approved and on the operating table. Follow your pre-op diet.
 A large liver prevents your surgeon from visualizing certain anatomy during the procedure. If the liver is too large, it then becomes unsafe to perform your gastric bypass surgery. Surgery may then be canceled and rescheduled to a later date.
A large liver prevents your surgeon from visualizing certain anatomy during the procedure. If the liver is too large, it then becomes unsafe to perform your gastric bypass surgery. Surgery may then be canceled and rescheduled to a later date.
The 1-2 week pre-op diet will include the following elements:
- Protein shakes or meal replacement shakes will be the diet's primary component.
- Only sugar-free beverages are allowed (sugar substitutes are okay).
- No caffeinated or carbonated beverages are permitted.
- Soup broth with no solid pieces of food may be consumed.
- V8 and vegetable juice are acceptable.
- Extremely thin cream of wheat or cream of rice may also be eaten.
- One or two daily servings of lean meat and/or vegetables might be okay, but only if they are approved by your surgeon or registered dietician.
All beverages and liquids should be sipped very slowly. Beverages should not be consumed with meals, and the patient should wait at least 30 minutes after a meal before consuming any type of liquid.
Separating your liquids and solids applies post-operatively (after surgery) but it's a good habit to start pre-operatively.
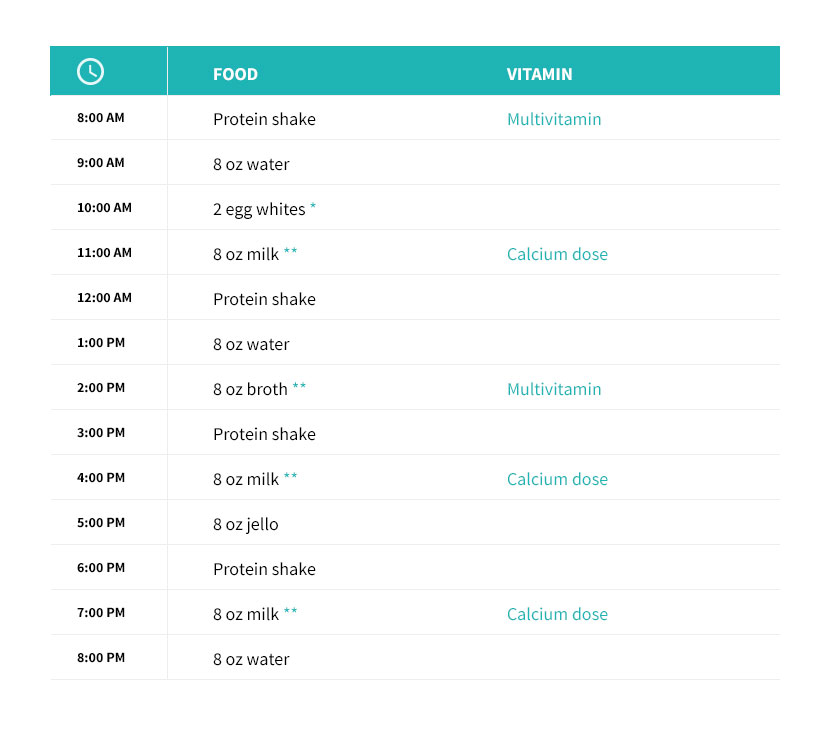
A daily meal plan for the patient's pre-op liquid diet may look like this:
High Protein Meal Replacements
During the pre-op phase (prior to surgery) your body will go into ketosis. This allows your body to use your fat stores as an energy source. The result is the fat in your liver shrinks considerably in a short amount of time. As seen above, your diet is high in protein and low in carbohydrates. Below are some suggested high protein meal replacements:
- Bariatric Advantage
- EAS Myoplex Light/Carb Control
- Isopure
- Unjury
- Chike
- GNC Total Lean Shake 25
Notes Pre-Op
Talk to your doctor about stopping certain medications prior to surgery. The following medications are typically stopped 1 week prior to surgery and may require tapering down the dose.
- Coumadin
- Steroids
- Other anti-coagulation medications
- Aspirin, Motrin, Advil, Celebrex, and any other NSAIDs
- Replacement hormones
- Birth control
If you have sleep apnea and use a CPAP machine, plan on bringing it to the hospital. Purchase vitamins and supplements in advance of surgery. Find a good protein shake.
If you smoke you should stop prior to surgery. Smoker's have an increased risk of blood clots and complications during and after surgery. Make a plan and implement it a few weeks prior to surgery.
- Resist the "Last Supper Syndrome." An empty stomach is easier to work with.
- Don't eat or drink anything on the day of surgery (typically, starting at midnight the night before).
Post-Op Dietary Guidelines
Once gastric bypass surgery is complete, a strict post-op diet plan needs to be followed. There is now a staple line in your stomach that must be allowed to heal. Certain foods can disrupt the healing process, put undue stress on the staple line, and lead to a leak.
The diet for a post-op gastric bypass patient consists of four stages:
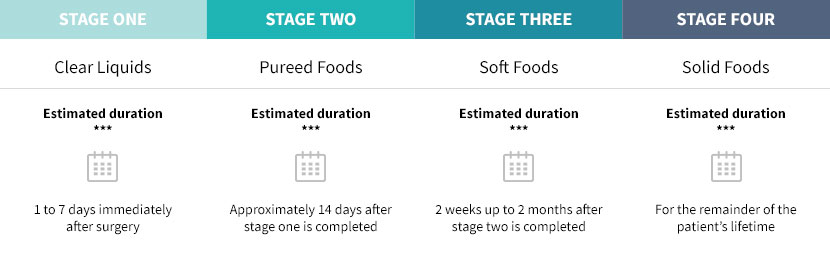
Week 1 – Clear Liquids
For 1 to 7 days after gastric bypass surgery, only clear liquids are to be consumed at the rate of one to two ounces per hour. The patient's dietitian will decide how long this phase will last and suggest dietary guidelines.
Clear liquids recommended by the dietitian will probably include the following items:
- water
- fat-free milk
- fat-free broth
- sugar-free Jello
A stage one clear liquid consumption schedule might look like this:
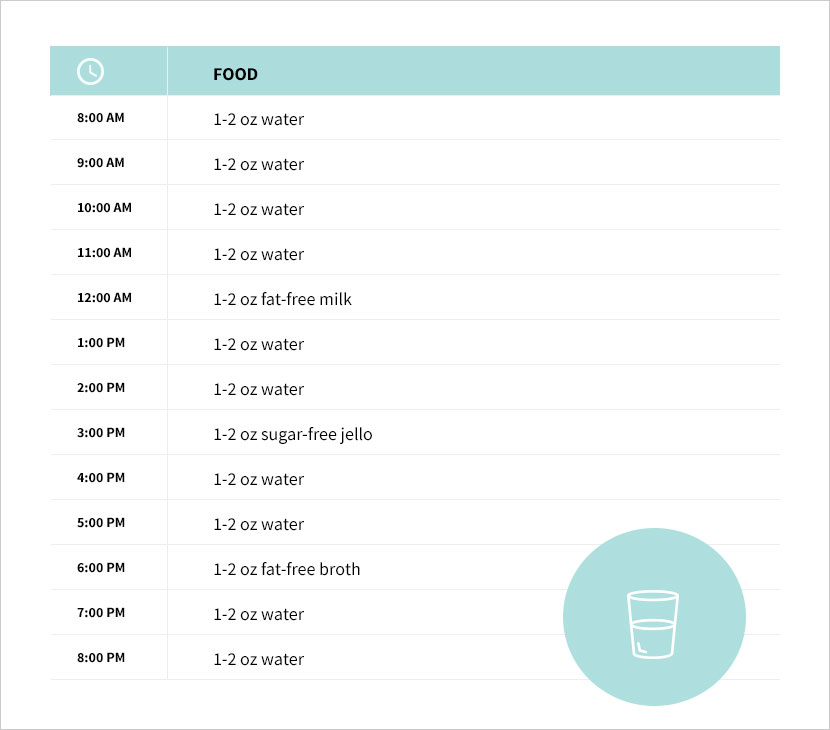
During this phase, it's important to stay hydrated. Some surgeons may want you to start protein shakes a few days after surgery. Follow your surgeon's guidelines.
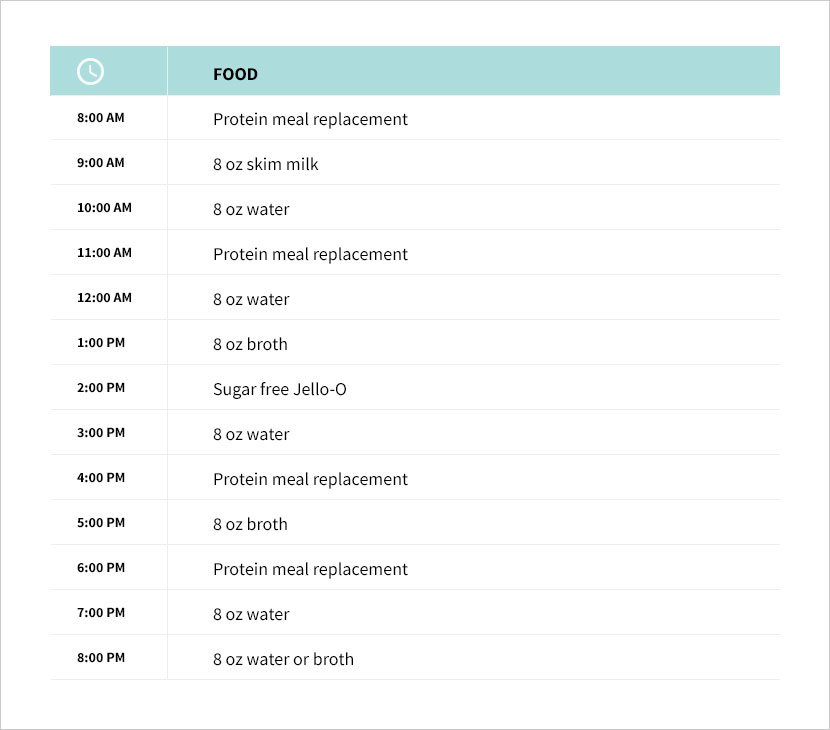
Week Two and Three – Pureed Foods and Protein Shakes
After 1 to 7 days of drinking clear liquids, you will be given permission to consume liquefied sources of protein. This stage of the post-op diet will usually last for one week (occasionally 2).
Because of the patient's smaller stomach size, the individual should have several smaller meals throughout the day. Your daily intake should be about 60-70 grams of protein (protein shakes, egg whites, pureed meat/fish) and approximately 64 ounces (about 8 glasses) of clear liquids (as defined in stage one) not counting the fluid in the pureed foods.
 Caffeinated and carbonated beverages should are not to be consumed. Refined sugars and simple carbohydrates (including sugar alcohol) should be avoided as well.
Caffeinated and carbonated beverages should are not to be consumed. Refined sugars and simple carbohydrates (including sugar alcohol) should be avoided as well.
Below is a list of the pureed protein sources that are typically allowed by the patient's dietitian or surgeon:
- Protein shakes
- Egg whites
- Non-fat soft cheese
- Non-fat cottage cheese
These food substances should be pureed with water, fat-free milk, or fat-free broth. Clear liquids (water) should not be consumed at the same time as the pureed foods. As a general guideline, it is usually suggested that the patient not drink any clear liquid 30 minutes before a meal and 60 minutes after a meal.
Clear liquids should be sipped very slowly, and straws should not be used because they might bring unwanted air into the stomach.
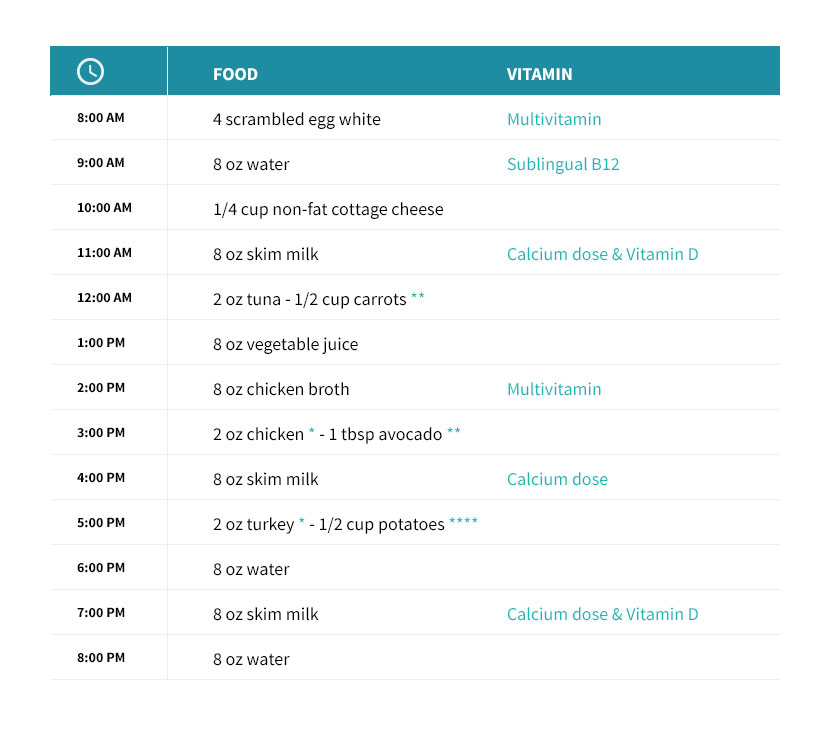
It is necessary to take one or two multivitamins (containing iron) every day in order to prevent nutrient deficiencies. The multivitamins should be in chewable or liquid form.
It is also important to supplement your diet with calcium citrate; the recommended amount will usually be two or three doses with each dose ranging from 400 mg to 600 mg. C alcium citrate supplementation should be separated from the multivitamin dosages by at least two hours . This is because iron and calcium can interfere with each others absorption.
A stage two meal plan might look like this:
Week 4 and 5 – Soft Foods
This stage of the diet will allow for a very gradual reintroduction of soft foods into your diet. This stage usually lasts about 1 or 2 weeks.
If a food can be easily mashed with a fork, knife, or a spoon, then it is a candidate for stage three of the post-op gastric bypass diet. This portion of the diet will include soft meats and cooked vegetables.
The nutrient goals will remain the same as in stage two. 60-70 grams of protein and 64 ounces of fluid is recommended daily. The serving size of protein in stage three should be about 1 to 2 ounces and you'll likely have 3 to 6 small meals.
[pullquote type="left, right"]Stage three, like stage two, focuses on high-quality lean protein sources. [/pullquote]While stage 3 continues to focus on high-quality lean protein sources, up to three servings of soft vegetables may also be allowed; a tiny portion of fat may also be permitted (this small portion of fat will probably be from a single serving of ripe avocado).
Recommendations for the protein sources in this stage of the diet will probably include several of the following items:
Meat, Dairy, and Eggs
- lean chicken
- lean turkey
- fish
- egg whites
- non-fat cottage cheese
- non-fat cheese
- tofu
Vegetables
- potatoes
- carrots
- green beans
- tomatoes
- squash
- cucumbers
- bananas
- avocados
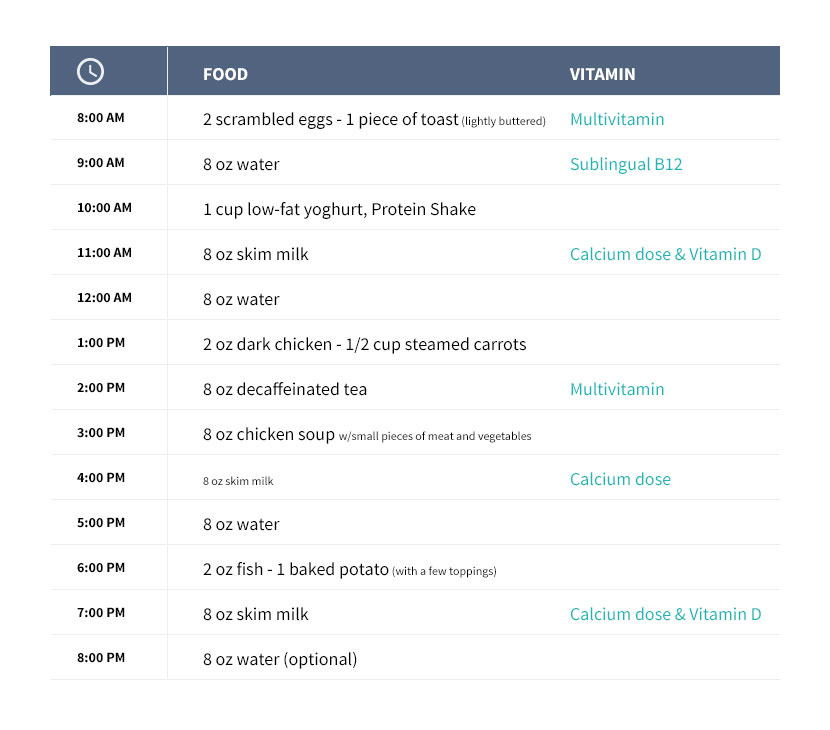
You will still need two multivitamins and two to three 400-600 mg doses of calcium citrate (with each of these doses to be taken at least two hours apart from each other).
Your dietitian may recommend you take 1,000 IU of Vitamin D3 per day; this will most likely be divided into two 500 IU doses. These should be taken with your calcium citrate. Also, a daily dose of sublingual B12 (500-1,000 mcg) may be recommended. A weekly or monthly injection or intranasal option may be available for B12. Some dietitians may want you to begin vitamin D3 and B12 supplementation in stage two.
This is what a typical stage three meal plan might look like:
* finely diced and moist / ** boiled or steamed until very soft / *** must be ripe enough to be soft / **** mashed
Week 6 – Solid Foods
Solid food is back! You've made it this far and it's time to start eating real food. This does not mean you get to eat whatever you want.
 A diet consisting of protein, vegetables, a limited amount of grains, and very little, if any, refined sugars should be followed for the rest of your life.
A diet consisting of protein, vegetables, a limited amount of grains, and very little, if any, refined sugars should be followed for the rest of your life.
Tips for starting solid foods:
- Introduce one new food at a time; ideally not more than one new food a day so you can gauge your body's reaction.
- Eat slowly. Chew your food well, 15 seconds each bite. Use the timer on the Baritastic app.
- Separate your food and water by at least 30 minutes.
- Continue to drink at least 64 ounces of water a day.
- Eat your protein first, vegetables second and carbohydrates third (ideally healthy grains and/or fruits, not processed foods).
- Eat real nutrient dense foods. Stay away from pre-packaged and processed foods with a lot of ingredients.
- Read labels. Focus on foods low in carbohydrates and a calorie to protein ratio of 10 to 1 or less (add a zero to the grams of protein and if the total calories are more than that then you may want to avoid that food – particularly if you are struggling to reach your protein goals).
Dumping syndrome occurs when sweet and/or fatty foods have been consumed too quickly or in too large a quantity. The stomach dumps the food into the small intestine before it's properly broken down. Dumping syndrome usually causes nauseousness, cramping, diarrhea, sweating, vomiting, or an increase in heart rate; these symptoms usually wear off after one or two hours. But the experience of 'dumping' is very unpleasant and you'll want to avoid it.
To reduce the risk of dumping:
- Avoid high sugar/refined carbohydrate foods.
- Eat very slowly.
- Chew your food well.
Certain foods are very difficult to digest and should be approached with caution:
- beef
- pork
- shellfish
- grapes
- nuts
- whole grains
- corn
- beans
Basically, the same guidelines found in stage three will be carried over into this fourth and final stage of the patient's post-op dietary plan. The protein intake, vitamin supplementation, and clear liquid requirements remain the same.
More fruits and vegetables (both cooked and raw) may now be carefully added to your diet. Small amounts of fat and very small amounts of sugar may now be added with caution. Carbonated and caffeinated beverages may now be consumed in moderation.
The total caloric intake per day will usually range from 800 to 1,200 and up to 1,500 18 months after surgery.
A stage four meal plan would look like this:
Physical Activity And Exercise
It's time to start exercising. Actually, you should have started on stage 2. Walking, running, biking, weight lifting, aerobics, canoeing, badminton, hiking, and dancing in your bedroom like a crazy person can all be added to your weekly routine. Ensure that you are getting at least 30 minutes of exercise 5 to 7 days a week. It doesn't matter how you do it, just do it.
Note: Do not lift more than 10 pounds for at least 6 weeks after surgery. This can put undue pressure on your internal stitches and result in a hernia.
Choosing Gastric Bypass Appropriate Foods
In general, you'll want to choose foods that are high to moderate in protein, low in carbohydrates and moderate in good fats.
Foods with good (healthy) fats include:
- avocados
- salmon
- nuts
- sardines
- nut butters
- coconut oil
General guidelines include:
- Choose lean meats.
- Canned tuna and salmon.
- Avoid greasy and spicy foods.
- Avoid whole milk.
- Eat nutrient dense foods (whole fruits, vegetables, meats, eggs).
- Plan your meals.
- Involve your family in healthy eating decisions.
- Shop for healthy foods.
- Limit or eliminate desserts.
- Don't tempt yourself with a pantry full of junk foods.
- Eliminate fast food.
- Eat out only on occasion.
- Take quality nutritional supplements/vitamins.
- Separate your water and food by at least 30 minutes.
- Introduce new foods slowly.
- Each meal should be no larger than your fist.
Recommended Articles
Your diet needs to change drastically after gastric bypass surgery. You should become an expert on healthy eating. Remember, the surgery will get the weight off but it's up to you to keep it off.
To calculate your expected weight loss after gastric bypass surgery, use our calculator.
- 5 Tips To Prevent Stretching Your Stomach After Gastric Bypass
- Before and After Interviews
- Bariatric Surgery – Which Procedure is Best?
CONCLUSION
Gastric bypass is one of the safest and most effective forms of weight loss surgery. For this reason, it is often referred to as the "gold standard."
You will lose weight with gastric bypass surgery – on average 70% of your excess weight. However, it's up to you to keep the weight off.
Follow your surgeon's diet guidelines, exercise 5 to 7 times a week for at least 30 minutes, and choose nutrient-dense non-processed foods. You will keep the weight off, reduce medications, become healthier, and live a longer, happier life.
For more information about gastric bypass surgery, check out our Expert's Guide To Gastric Bypass.
Diet Plan for Gastric Bypass Patients
Source: https://www.obesitycoverage.com/the-big-gastric-bypass-diet-guide/